Imagine a cough that just won’t go away, coupled with persistent fatigue that saps your energy. For one individual in Tanzania, these symptoms masked a far more sinister threat: drug-resistant tuberculosis, often described as Multidrug Resistant TB(MDR-TB).
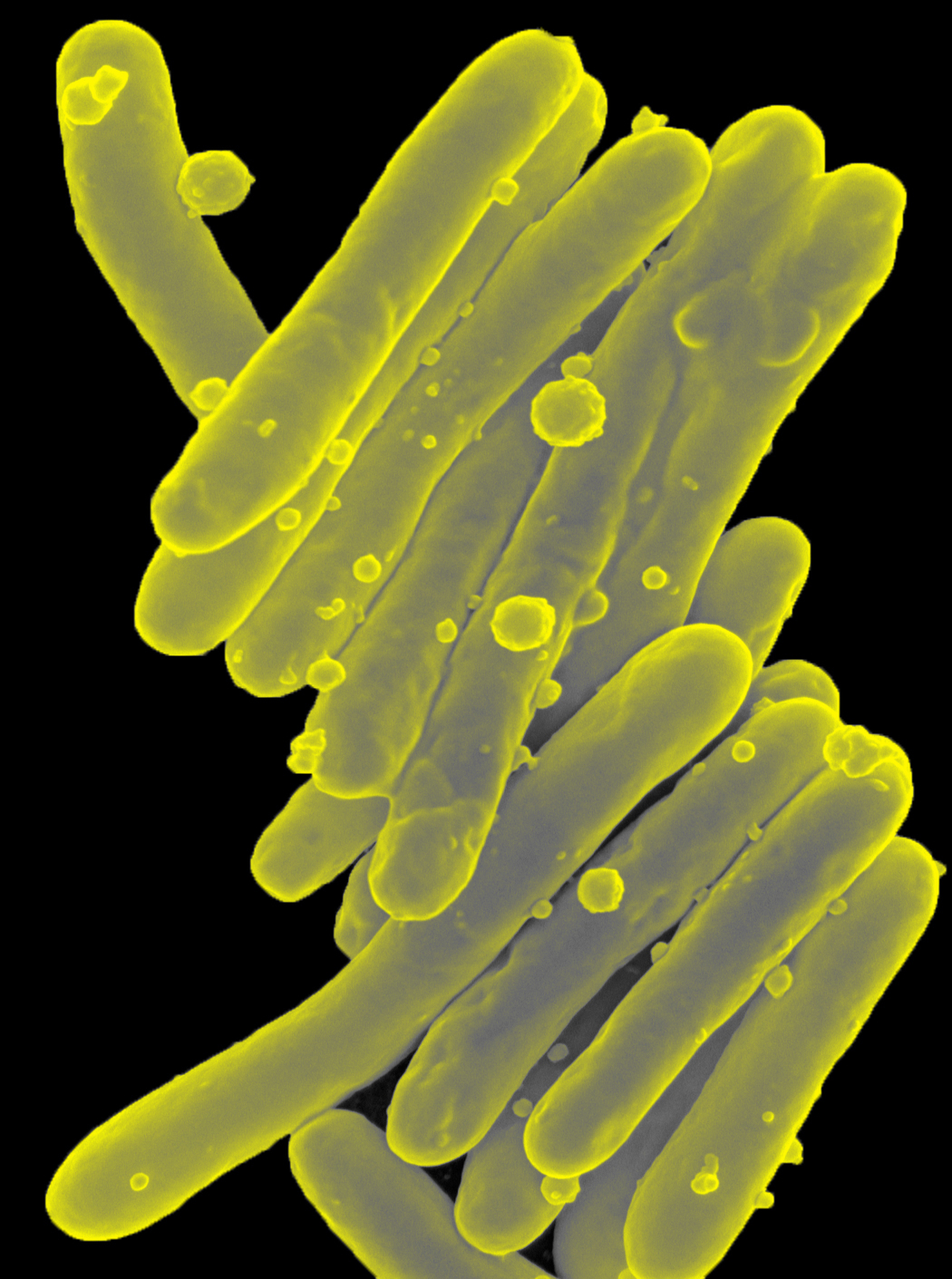
For starters, Tuberculosis (TB) is a serious lung disease caused by a bacterium called Mycobacterium tuberculosis. While often treatable with antibiotics, some forms have evolved resistance to these medications, creating drug-resistant TB. This resistance typically develops when bacteria mutate, rendering standard antibiotics ineffective. This can occur when individuals do not adhere to their prescribed treatment regimens or discontinue treatment prematurely. The most severe form, XDR-TB, exhibits resistance to multiple drugs, making it exceptionally challenging to cure. The human cost is immense, with individuals facing prolonged illness, diminished quality of life, and an increased risk of death. Furthermore, drug-resistant TB strains pose a significant threat to public health, as they can spread readily within communities, jeopardizing the health of others.
This patient from Tanzania began treatment for this form of TB, which is resistant to some of our most powerful antibiotics. But the battle was far from over. Due to the challenges of adhering to a complex and lengthy treatment regimen, the bacteria in the patient’s body evolved, becoming resistant to even more drugs, ultimately leading to extensively drug-resistant TB (XDR-TB). Heartbreaking as it sounds, this story is not just an isolated incident; it’s a microcosm of a global crisis which underscores a critical public health challenge: the rise of drug-resistant tuberculosis, a silent killer that threatens global health security.
This case from Tanzania serves as a stark reminder of the devastating consequences of inconsistent treatment and the urgent need for innovative diagnostic tools and personalized treatment strategies. It also highlights the power of modern genetic technology in our fight against this deadly disease.
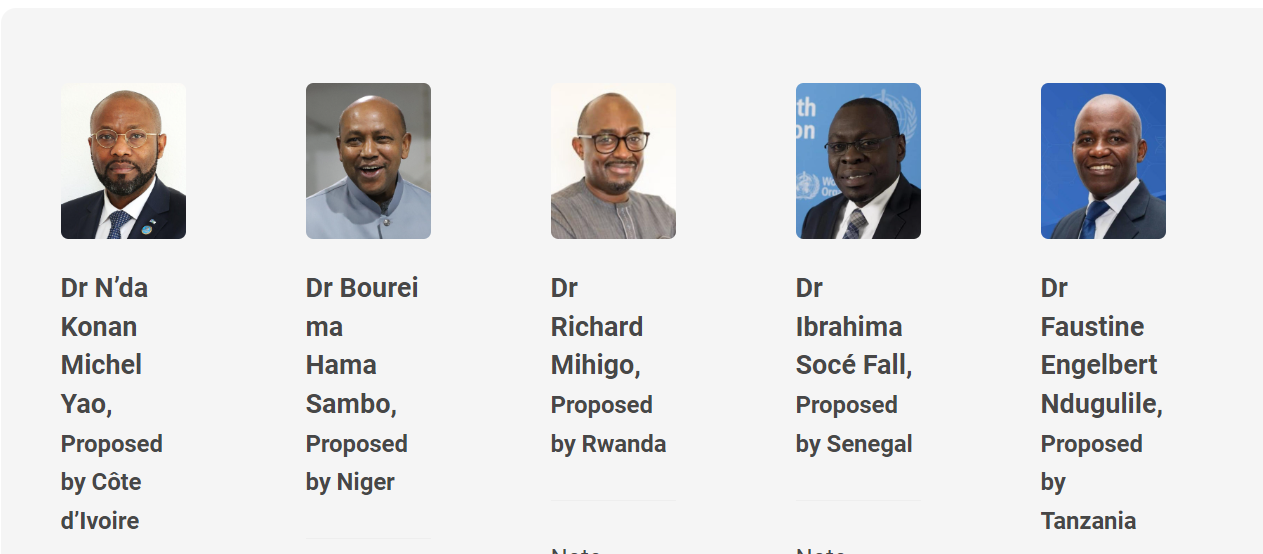
We investigated drug resistance mutations in a 32-year-old Tanzanian male admitted to Kibong’oto Infectious Diseases Hospital, and the findings have been published in the Annals of Clinical Microbiology and Antimicrobials. This work was done in collaboration with Tanzanian and international scientists. This study investigated a specific case of XDR-TB in Tanzania, employing advanced genetic testing to unravel the complexities of drug resistance and inform treatment strategies. The patient’s journey, from initially diagnosed MDR-TB to the more intractable XDR-TB, highlighted the critical role of treatment adherence in preventing the development of drug resistance. Our research sought to understand not only the clinical progression of the disease but also the evolutionary changes in the bacteria itself – a feat made possible by the power of modern genetic technology.
Our investigation revealed that the bacteria isolated from the patient belonged to the Beijing strain, a particularly virulent strain known for its rapid spread and association with poor treatment outcomes. While this strain is not widespread in Tanzania, its presence underscores the need for vigilance and robust surveillance systems. We compared two methods for assessing drug resistance: the conventional phenotypic drug susceptibility test (DST) and whole genome sequencing (WGS), a cutting-edge genetic technology.
While both methods largely concurred, discrepancies arose, particularly with newer drugs like bedaquiline and levofloxacin. These discrepancies likely reflect subtle genetic mutations within the bacteria that confer resistance, mutations that WGS is better equipped to detect. This ability to pinpoint specific genetic changes is where the power of modern genetic technology truly shines.
A crucial finding of our case report was the identification of specific mutations in the patient’s bacteria that conferred resistance to bedaquiline and clofazimine. Alarmingly, these mutations were present even before the patient had received these drugs. This suggests that bacteria can develop resistance to even newer drugs like bedaquiline, highlighting the relentless adaptability of these microorganisms and the need for careful monitoring of drug efficacy. The patient’s transfer to a different healthcare facility after treatment failure suggests a lapse in treatment adherence, further contributing to the development of drug resistance. The emergence of bedaquiline resistance in later samples, despite the absence of clofazimine resistance in earlier samples, underscores the importance of real-time monitoring of drug resistance evolution using advanced techniques like WGS. Without the power of modern genetic technology, these crucial insights into the bacterial evolution and the development of drug resistance would have remained hidden.
Managing XDR-TB presents a big challenge. Treatment options are limited, and the risk of transmission to others is high. This makes early detection of drug resistance, particularly to newer drugs like bedaquiline, and rigorous infection control measures paramount. Our study emphasizes the critical role of WGS in guiding treatment decisions. While the cost and expertise required for WGS may be significant, the detailed insights into bacterial evolution and drug resistance it provides are invaluable for optimizing treatment strategies and improving patient outcomes. This case from Tanzania demonstrates the transformative potential of modern genetic technology in combating XDR-TB. By investing in improved diagnostics and personalized treatment approaches, driven by the insights gained from WGS, we can make significant strides towards controlling and ultimately eliminating this devastating disease.
The fight against drug-resistant TB requires a multi-pronged approach. First and foremost, ensuring treatment adherence is critical. This requires not only providing access to medication but also addressing the social and economic factors that can hinder adherence, such as poverty, stigma, and lack of access to healthcare support. Second, strengthening diagnostic capacity, including wider access to WGS, is crucial for timely and accurate detection of drug resistance. Third, developing new drugs and treatment regimens is essential to stay ahead of the evolving resistance landscape. Finally, robust public health infrastructure and surveillance systems are needed to monitor the spread of drug-resistant TB and implement effective control measures. The case of the Tanzanian patient serves as a call to action. We must invest in the tools and strategies, including the continued advancement and application of modern genetic technology, necessary to combat drug-resistant TB, not only to save lives but also to safeguard global health security.