For 15 years, Dr. Siana Nkya, a biomedical scientist, has been studying how the building blocks of life—the genes and molecules—can be used to prevent, diagnose, monitor and treat diseases. Her focus is on developing new drugs and genetic therapies, and understanding how they work in different people—more so among patients with Sickle Cell Disease (SCD).
Beyond her role as a senior lecturer in Biochemistry and Molecular Biology at Muhimbili University of Health and Allied Sciences (MUHAS), Dr. Nkya has been actively engaged in international collaborations with prestigious institutions such as King’s College London, the Wellcome Trust Sanger Institute, Boston Children’s Hospital, and the University of Northumbria, all with the aim of advancing our understanding diseases and explore potential treatments, particularly malaria and sickle cell disease and explore potential treatments.
The switch
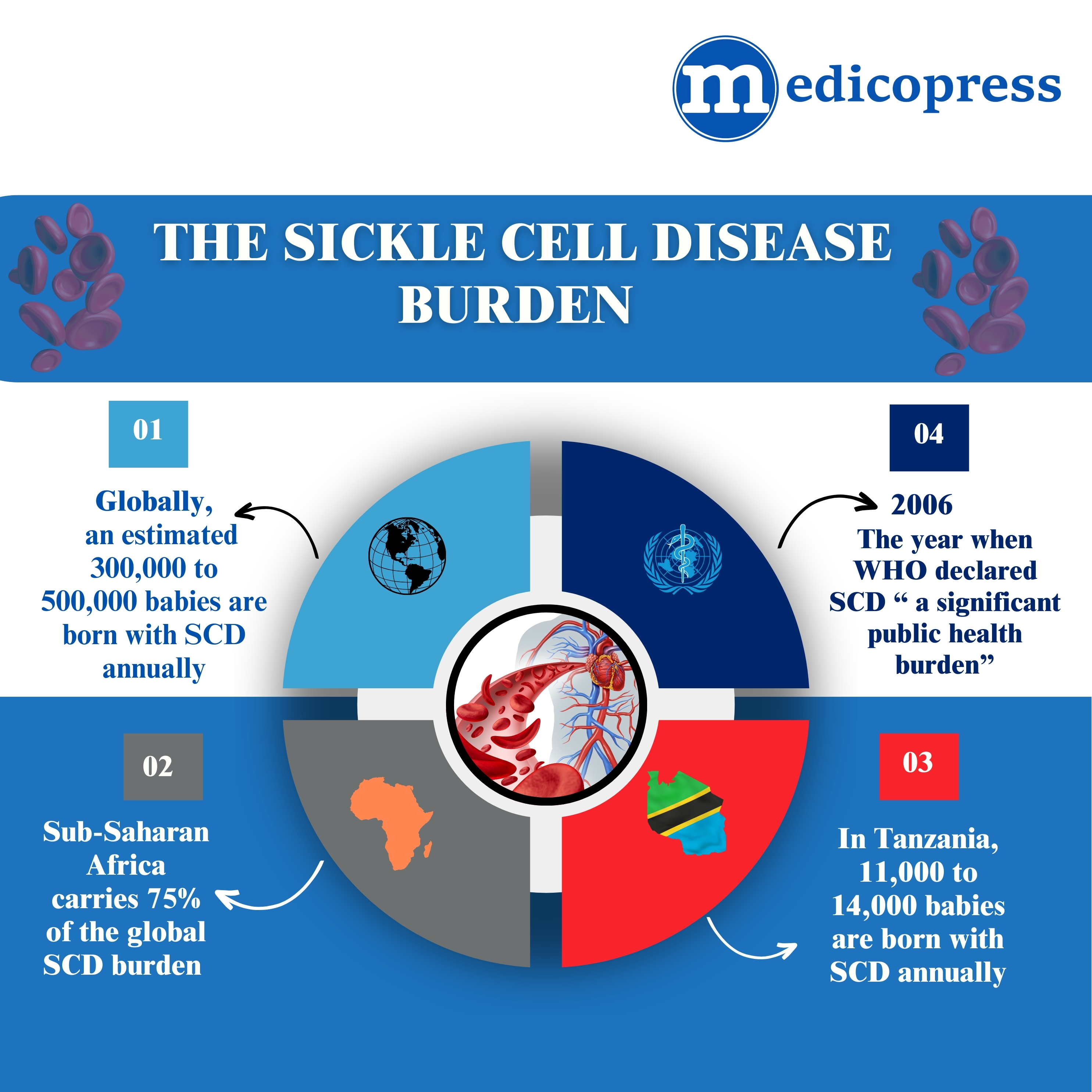
You are about to delve into some of the life-saving science phenomena that Dr. Nkya has dedicated her career to researching, particularly in SCD, with Sub-Saharan Africa carrying the heaviest disease burden.
And just a glimpse into some interesting science facts that make Dr. Nkya’s story fascinating: Do you know what fetal hemoglobin (HbF) is? It’s a special protein that transports oxygen from a mother to her unborn baby through the placenta. At birth, about 85% of a baby’s hemoglobin is HbF, but this level rapidly declines within a year to below 1% as the body SWITCHES to producing adult hemoglobin (HbA). This natural process is a key focus of Dr. Nkya’s recent research.
For scientists such as Dr. Nkya, the SWITCH from fetal to adult to haemoglobin is key for development of relevant drugs and therapies that may save the lives of children with SCD.
“This switch can be a lifesaver and has been extensively studied with a focus of developing SCD interventions’’
Dr. Siana Nkya, BSc, MSc, PhD, Senior Lecturer-Muhimbili University of Health and Allied Sciences(MUHAS)
Dr. Nkya, a former Fogarty Global Health Fellow, has recently completed a five-year project funded by the US-based National Institutes of Health (NIHI), where she followed over 250 infants, both with and without sickle cell disease, to understand how their bodies switch from fetal to adult hemoglobin.
This research revealed that infants with sickle cell disease experience a slower decline in fetal hemoglobin, compared to their counterparts, probably as a protective mechanism. As part of this study, Dr Nkya is tackling the complex question of how the decline of this fetal hemoglobin affects infants with sickle cell disease, alongside determining the genetic factors involved in this process.
“Such studies are important especially in the Sub-Saharan Africa population where the highest burden of the disease is,’’ she told MedicoPRESS.
By understanding the genetic factors that influence the switch, scientists like Dr. Nkya are working to develop treatments like hydroxyurea, which can help to synthesize fetal hemoglobin and improve the lives of people with sickle cell disease.
What does hydroxyurea do?
This medication works by increasing the production of fetal hemoglobin (HbF), a type of hemoglobin that is more flexible and less likely to sickle. This increased HbF helps prevent the painful crises and organ damage associated with SCD.This is the only available medication that is known to reinstate the synthesis of fetal hemoglobin to levels that are protective for individuals with SCD. The increased levels of fetal hemoglobin counterfeit the damages that are brought by the sickle hemoglobin S.
What controls the switch?
“The switch is to a great extent controlled by genetic factors,” explains Dr. Nkya. This genetic control allows for the timely expression of different hemoglobin subtypes. One such genetic factor, BCL11A, is now being targeted by innovative gene therapies.
A successful switch to fetal hemoglobin production can prevent the manifestation of sickle cell disease. This is because fetal hemoglobin interferes with the process that leads to sickle cell formation, reducing the risk of blocked blood vessels and pain.
Dr. Nkya has been collaborating with researchers in Ghana and Nigeria to explore the role of genetic factors on hydroxyurea treatment outcomes.

She says that alternative therapies for Sickle Cell Disease are on the rise. For example, two out of eleven gene-based therapies received approval by December 2023. Similarly, more than three molecules/drugs are at different stages of trials and approval. It’s crucial to predict treatment outcomes early on so as to direct patients toward the most suitable treatment options.
Dr. Nkya highlights the promising rise of alternative therapies for Sickle Cell Disease, pointing out that as of December 2023, two out of eleven gene-based therapies have received approval. Additionally, over three molecules or drugs are currently undergoing trials and the approval process. Based on these facts, she emphasizes on the need to predict treatment outcomes early on so as to direct patients toward the most suitable treatment options.
Nkya’s role in human genetics
Additionally, she is actively involved in the African Society of Human Genetics, where she advocates for increased investment in genetic research and education across the continent.
Her work has not only contributed to a better understanding of SCD but has also laid the groundwork for future research and policy development in genetics across Africa. It is now known that Africa is a genetics/genomics gold mine. This calls for the African countries and partners to ensure sustainable investments are in place including trained scientists and researchers, funding and centers of excellence. Scientists like Nkya are also obliged to mentor junior researchers
In fact, Nkya, who is president of the Tanzanian Human Genomics Organization (THGO), has been actively involved in advancing genetic research and policy in Tanzania. Under her leadership, THGO, which will soon celebrate its fifth anniversary, has made significant progress in advocacy, training, research, diagnosis, and therapeutics.