One in eight patients in hospitals across Africa is critically ill, with one in five of those patients dying within seven days, says a new study, suggesting a fundamental shift in how critical care is understood and delivered.
Many of these lives, say the researchers, could have been saved with access to cheap life-saving treatments.
The vast majority of the critically ill individuals are cared for in general wards and often deprived of essential emergency and critical care (EECC), reveals the study published in The Lancet, igniting calls for urgent action across the continent’s healthcare systems.
“Our findings should change the way we think about critical care,” says Dr. Tim Baker, Associate Professor at the Department of Global Public Health at Karolinska Institutet, the lead author of the study which involved nearly 20,000 patients in 180 hospitals across 22 African nations.
But what does being critically ill mean? It means having severely affected vital functions, such as extremely low blood pressure or low levels of oxygen in the blood. In the context of the study, this translates to patients arriving at overwhelmed hospitals with conditions that, while critical, are often treatable with basic interventions, but without those interventions, they quickly deteriorate and die.
“There is a much larger burden of critical illness than we previously thought. Simple, low-cost, essential emergency and critical care is not being provided. Many deaths are preventable,’’
Dr. Tim Baker, Associate Professor at the Department of Global Public Health at Karolinska Institutet
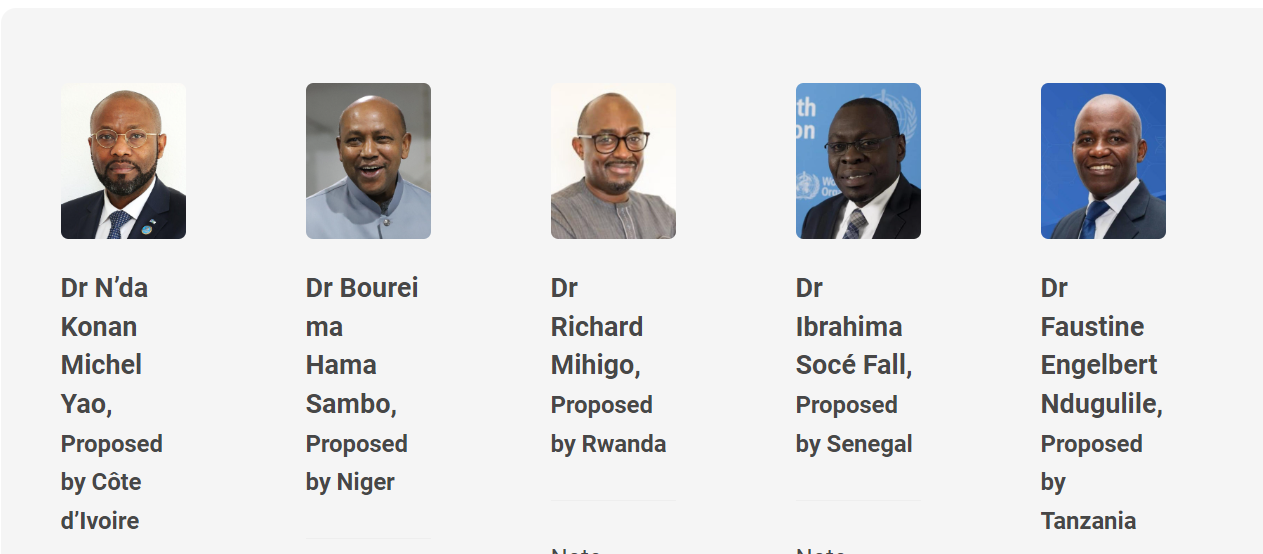
Tanzania is one of the key locations for the study, which was funded by the National Institute for Health and Care Research (NIHR). It’s a collaboration between Karolinska Institutet and universities in South Africa, Tanzania, Ethiopia, Uganda, and the UK.
Data obtained shows that 12.5% of adult inpatients are in a state of critical illness, defined by severely compromised vital functions like dangerously low blood pressure or oxygen levels.
“But there is hope,’’ says Dr. Karima Khalid, lecturer at Muhimbili University of Health and Allied Sciences (MUHAS), highlighting the prevalence—far higher than previously recognized.
Despite the immense burden placed on African hospitals, there is “a huge potential to save lives through essential emergency and critical care (EECC),” as explained by Dr Khalid, a PhD candidate who has studied EECC—a potentially transformative approach to critical care in resource-constrained settings.
The researchers have found that across many hospitals in Africa, critically ill patients deteriorate in general wards, not ICUs. When a patient deteriorates, frantic attempts to secure an ICU bed often fail, leaving them without vital interventions.
“If all patients had access to essential emergency and critical care, we could significantly reduce mortality. Moreover, these interventions are inexpensive and can be provided in general wards,” says Carl Otto Schell, researcher at the Department of Global Public Health at Karolinska Institutet and one of the initiators of the study.
A shift towards EECC within general wards offers a lifeline for the patients. By training staff in basic life support and equipping wards with essential tools, hospitals can stabilize the patients on the spot, reserving precious ICU beds for only the most complex cases, thus saving more lives.
The study further found a 21% mortality rate among these critically ill patients within a week, a stark contrast to the 2.7% mortality rate among non-critically ill patients.
Perhaps the most troubling finding is that 69% of these critically ill patients are being treated in general wards, not in specialized intensive care units (ICUs). This reliance on general wards, coupled with the fact that 56% of critically ill patients do not receive even the most basic EECC, such as oxygen therapy, intravenous fluids, or airway management, underscores a systemic failure.
The researchers emphasize that these are not complex, expensive interventions; they are fundamental, life-saving treatments that can be administered in standard hospital settings.
The interventions highlighted in the study, such as oxygen therapy and fluid resuscitation, are relatively inexpensive and can be easily integrated into existing hospital infrastructure.
The researchers say affordability makes EECC a viable strategy for improving critical care outcomes in resource-limited settings and the study provides concrete evidence to inform policy and resource allocation, demonstrating that investing in EECC training, process changes, and implementation programs can yield significant returns in terms of lives saved.